Author :-Mr. Zeeshan Fayaz .
Clinical Pharmacologist & Toxicology ,
Certified Mental Health Counselor ,
Member of American clinical Pharmacological Society ,
Member of Indian Pharmacological Society (IPS).
Abstract
Inhalation therapy is the cornerstone of management for chronic respiratory diseases such as asthma and chronic obstructive pulmonary disease (COPD). Inhalers provide targeted drug delivery to the lungs, ensuring rapid onset of action with minimal systemic side effects. Despite their proven efficacy, incorrect inhaler technique and prevalent misconceptions significantly compromise treatment outcomes. This review highlights the proper use of inhalers, their clinical benefits, and addresses common myths, emphasizing the role of healthcare professionals in patient education to optimize therapeutic effectiveness.
Introduction
Asthma and chronic obstructive pulmonary disease (COPD) are among the most common chronic respiratory disorders worldwide, contributing substantially to morbidity and healthcare burden. Inhaled medications form the backbone of treatment as they deliver drugs directly to the site of disease. However, studies indicate that a significant proportion of patients fail to use inhalers correctly, resulting in poor disease control, frequent exacerbations, and increased healthcare utilization. This article reviews inhaler types, correct usage, clinical benefits, and common myths associated with inhaler therapy.
Types of Inhalers
Inhalation devices are broadly categorized into:
-
Metered Dose Inhalers (MDIs):
Deliver a fixed dose of aerosolized medication using a propellant. -
Dry Powder Inhalers (DPIs):
Require sufficient inspiratory effort to disperse powdered medication. -
Soft Mist Inhalers (SMIs):
Generate a slow-moving mist improving lung deposition. -
Nebulizers:
Convert liquid medication into aerosol; commonly used in pediatric, geriatric, or severe cases.
Each device has a unique technique, and incorrect usage significantly reduces lung deposition.
Proper Technique for Inhaler Use
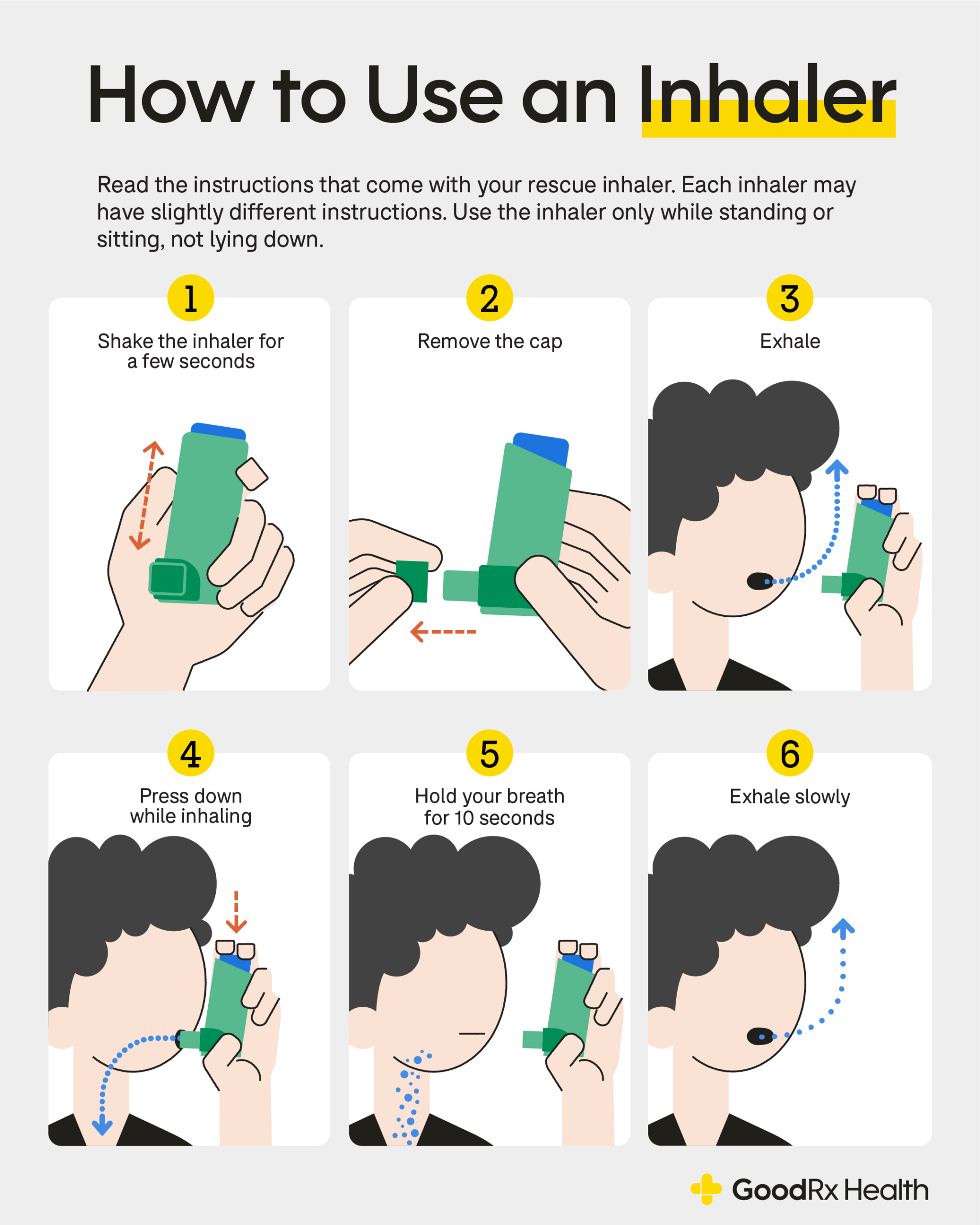
Metered Dose Inhalers (MDIs)
-
Remove the cap and shake the inhaler.
-
Exhale fully.
-
Place the mouthpiece between lips with a tight seal.
-
Begin slow inhalation and actuate the inhaler simultaneously.
-
Continue inhaling deeply for 3–5 seconds.
-
Hold breath for 8–10 seconds.
-
Exhale slowly.
-
Repeat dose after 30 seconds if prescribed.
-
Rinse mouth after inhaled corticosteroids.
Use of a spacer device is recommended to enhance drug delivery and minimize oropharyngeal deposition.
Benefits of Inhaler Therapy
-
Targeted pulmonary drug delivery
-
Rapid onset of action
-
Lower systemic adverse effects
-
Reduced required drug dosage
-
Improved symptom control and lung function
-
Safe for long-term use
These advantages make inhalers superior to oral therapy in most chronic respiratory conditions.
Common Myths and Misconceptions
Myth 1: Inhalers are addictive
Fact: Inhalers are not addictive; they are essential for controlling airway inflammation and bronchospasm.
Myth 2: Inhalers are only for severe disease
Fact: Early initiation prevents disease progression and exacerbations.
Myth 3: Oral medications are more effective
Fact: Inhaled medications are more effective due to direct lung delivery.
Myth 4: Inhaled steroids are dangerous
Fact: Inhaled corticosteroids are safe at prescribed doses with minimal systemic effects.
Myth 5: Inhalers can be stopped once symptoms improve
Fact: Discontinuation without medical advice increases relapse risk.
Consequences of Incorrect Inhaler Use
Improper inhaler technique is associated with:
-
Poor disease control
-
Increased exacerbations
-
Unnecessary escalation of therapy
-
Increased healthcare costs
-
Reduced patient adherence
Studies show that over half of patients demonstrate incorrect inhaler technique even after prior instruction.
Role of Healthcare Professionals
Healthcare providers must:
-
Demonstrate correct inhaler technique
-
Reassess technique during follow-up visits
-
Address patient concerns and misconceptions
-
Reinforce adherence and correct usage regularly
Repeated education significantly improves inhaler technique and clinical outcomes.
Conclusion
Inhalers remain the cornerstone of asthma and COPD management. Their clinical effectiveness depends heavily on proper technique and patient understanding. Dispelling myths and reinforcing correct inhaler use through continuous education can substantially improve disease control, reduce complications, and enhance patient quality of life.
References (Vancouver Style)
-
Global Initiative for Asthma (GINA). Global Strategy for Asthma Management and Prevention. 2023 Update.
-
Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global Strategy for the Diagnosis, Management, and Prevention of COPD. 2023 Report.
-
Lavorini F, Magnan A, Dubus JC, et al. Effect of incorrect inhaler technique on management of patients with asthma and COPD. Respir Med. 2008;102(4):593–604.
-
Melani AS, Bonavia M, Cilenti V, et al. Inhaler mishandling remains common in real life and is associated with reduced disease control. Respir Med. 2011;105(6):930–938.
-
Basheti IA, Reddel HK, Armour CL, Bosnic-Anticevich SZ. Improved asthma outcomes with a simple inhaler technique intervention. Respir Care. 2007;52(10):1290–1298.
-
Newman SP. Principles of metered-dose inhaler design. Respir Care. 2005;50(9):1177–1190.
-
Barnes PJ. Inhaled corticosteroids. Pharmacol Ther. 1998;58(1):29–43.
Case studies available upon request.
Please provide information on how we can help you and we will be in touch to help meet your requirements.